When I just started working as a specialist orthodontist, I would provide a lot of rapid maxillary expansion (RME) to my mixed dentition patients. Even in the absence of posterior crossbite. I would tell the parents that this will help the teeth to erupt in a better position. I would especially emphasise the potential problems with the permanent canines that I was hoping to prevent with the RME.
I would say and do this because I hadn’t had enough clinical experience and wasn’t familiar with the research data on the subject. I also would probably want to impress the parents with my “comprehensive approach” expecting them to return for the second phase of treatment in a few years.
Today I still do RME in children in the absence of crossbite. But in the very particular situations. In this blog post, I want to look at some brilliant papers which helped me better understand the topics of the mixed dentition RME and canine impaction. Hopefully, it will be of benefit for some of my readers…
How do we traditionally prevent canine impaction?
First, I want to look at a classic paper from 1988 by two Swedish orthodontists, Sune Ericson and Jüri Kurol.
Early treatment of palatally erupting maxillary canines by extraction of the primary canines S. Ericson, J. Kurol, Eur J Orthod. 1988 Nov;10(4):283-95. doi: 10.1093/ejo/10.4.283.
In their study, the authors identified 35 individuals between 10 and 13 years with the palatally displaced maxillary canines (PDC). The authors showed that after the extraction of the primary canine, 36 of the 46 permanent canines (78%) changed their eruption pattern to normal.
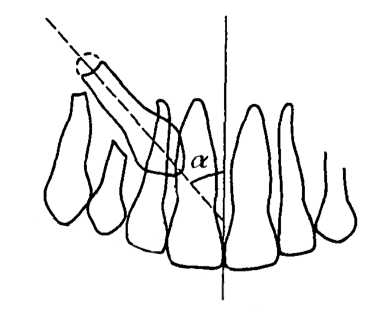
The authors also composed the diagrams (pictures 1 and 2) that can help us to predict and prevent eruption problems. Interestingly, all new studies, such as this by Julia Naoumova et al. from 2018, only reinforce the findings from 30 decades ago.
Picture 1. The higher the number of the sector is, the lesser the chance of the PDC to respond to the intervention. Canines in sector 1 are of little concern and should erupt in time. Canines in sector 2 and 3 could benefit from the timely intervention. Canines in sector 4 and 5 are not likely to respond to the intervention and should be exposed surgically.

Picture 2. This illustration shows the alpha angle. All the points from the previous picture are true if it is not greater than 21 degrees. If it is, the success rates are going down.
Another great paper on the subject of the PDC has been written by Coulter and Richardson in 1997.
Normal eruption of the maxillary canine quantified in three dimensions J. Coulter, A. Richardson, Eur J Orthod.1997 Apr;19(2):171-83. doi: 10.1093/ejo/19.2.171.
The authors examined the longitudinal radiographic records of 30 children: the x-rays were taken annually from the age of 5 to 15 years. The authors identified that between the ages of 5 and 9 years lateral movement of the upper permanent canine was small. The canines start moving buccally after 9 years, with the greatest amount occurring between 10 and 12 years. As a result, we can conclude that a radiographic investigation of the canine position prior the age of 9 is practically useless.
What about RME?
It seems that the extraction of primary canines is a viable method to tackle the PDC problem. But can RME provide any additional help?
In 2009 and 2011, Baccetti et al. published a series of papers on the effect of RME on the eruption patterns of maxillary canines. These studies have issues with blinding and randomisation, but this is still the best evidence on the subject we have so far.
I am going to look closer at their randomised controlled trial published in 2011.
An RCT on treatment of palatally displaced canines with RME and/or a transpalatal arch T. Baccetti, J. Sigler, J. McNamara, Eur J Orthod.2011 Dec;33(6):601-7. doi: 10.1093/ejo/cjq139.
The authors allocated patients into three groups:
- RME followed by placement of a transpalatal arch (TPA) and extraction of the primary canine
- Placement of a TPA and extraction of the primary canines
- Extraction of primary canine only
The authors report that successful eruption of permanent canines occurred in 32 out of 40 (80%) of the patients in the RME group, which was no different to those who had just received a TPA and extraction of the primary canine (19 out of 24 individuals, 79%).
Successful eruption also occurred in 15 out of 24 (63%) of those who had extraction of the primary canine only, compared with 8 out of 29 (28%) in the untreated control group.
Every clinician should interpret this data for oneself. My interpretation is that RME is rarely necessary. In the vast majority of the PDC cases, it is enough to extract primary canines and place a TPA. The exception are probably the cases where the displacement is severe (sector 3).
Obstructive sleep apnea
Another objective that some clinicians claim to pursue with RME is curing obstructive sleep apnea (OSA). I have recently published a blog post with my summary of the AAO white paper on OSA. I want to reiterate two relevant takeaway messages:
- The most common risk factors of OSA are hypertrophic tonsils/adenoids and obesity. As a result, these conditions should be addressed as the first line of treatment.
- There is some evidence that RME in mixed dentition cases can alleviate the symptoms of OSA both short and long term, however should not be used as prophylaxis.
Conclusion
I decided to write this blog post because I feel that today it becomes a norm for some orthodontic practices to indiscriminately take CBCT scans of children starting from the age of 7 or even earlier. This is often follows by an indiscriminate prescription of maxillary expanders which we now have in manyfold designs. The 3D images of the permanent dental follicles are often used to impress the parents: “Do you see that severe crowding your child has?” To a degree, this is done not to lose patients with an expectation to get them back at the age of 12.
As I wrote before, I had also been influenced by this trend in the very beginning of my career. Fortunately, I did’t have an access to a CBCT machine then. Ironically, very few of my “aimlessly expanded” patients have returned whereas those patients whom I provide limited and goal-orientated early treatment are coming back and referring friends very willingly.
Now I want to sum up my knowledge about RME and PDC in 7 simple points. I will also indicate some exceptional situations which, in my view, require RME without the absence of crossbite.
- Loading a child into a CBCT machine without a clear clinical justification is straightforwardly a malpractice. We shouldn’t expose our patients to unnecessary radiation.
- Most of the problems with the palatally displaced canines can be easily identified between a dental age of 10 and 12 years using conventional radiographs.
- Extraction of the primary canines looks like a viable method to normalise the eruption of the palatally displaced successors in most of the cases.
- Rapid maxillary expansion during the mixed dentition should not be provided indiscriminately for prophylaxis purposes. It might be justified by either OSA symptoms or severely displaced canines (sector 3). In the latter cases, RME should be provided together with the extraction of the primary canines to increase the success rate of the intervention.
- The exceptions are esthetic concerns due to severe crowding, and cases with a tapered maxilla accompanied by an increased Wilson curve in the mandible. I also don’t think this require taking a CBCT scan. An experienced clinician can easily tell a normal developing from a maxillary constriction.
- And, of course, we SHOULD expand cases with buccal crossbites. Doing so, we also have to achieve some degree of overcorrection. Because the soft tissues are going to partially reverse our work.
- You most likely have your patients back for the second phase treatment if you won’t overtreat them during the first phase. However, this is not an evidence-based statement.

Excellent. Enjoyed reading that. Thank you.
LikeLike
Hi David! Thanks for stopping by and leaving a comment!
LikeLike
Should we move it towards the arrow or to the opposite direction
LikeLike
Dear Alex,
eben if RME may enhance the eruption of a displaced canine the unanswered stays the same:
How to deal with the unwanted effect on the occlusion in case of absence skeletal transversal deficiency?
I think it’s not very smart to solve a small problem by creating a bigger one.
LikeLike
Hi Jassin, this is a good point. My feeling is that PDC issue and increased Wilson curve often go together. Other than that, I totally agree with you – we should not overcomplicate the situation.
LikeLike
[…] Should we rapidly expand children in the absence of crossbite? […]
LikeLike
Enjoyed reading this…
LikeLike
Thanks Theresa! It’s been 3 years since I wrote it but the topic is not getting obsolete…
LikeLike